Translational Perioperative and Pain Medicine (ISSN: 2330-4871)
ARTICLE DOI: 10.31480/2330-4871/122
Review Article OPEN ACCESS
Emergency Anesthesia in a Patient with Esophageal Foreign Matter Infected with COVID-19: A Case Report
Huan Tao1, Kai Yang1, Zheng Gan1, Fen Ouyang2, Shanglong Yao1, Weike Mao1* and Chengkun Xia1*
1Department of Anesthesiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430022, China
2Department of Operating Room, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430022, China
Weike Mao and Chengkun Xia, Department of Anesthesiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430022, China, Emails: Weike Ma: mweike@163.com; Chengkun Xia: xiayulong_2001@163.com
Editor: Renyu Liu, MD, PhD, Professor, Department of Anesthesiology and Critical Care, Perelman School of Medicine at the University of Pennsylvania, Center of Penn Global Health Scholar, Director of Stroke 120 Special Task Force, Chinese Stroke Association, 336 John Morgan Building, 3620 Hamilton Walk, Philadelphia, PA 19104, USA, Phone: 2157461485, Fax: 2153495078, E-mail: RenYu.Liu@pennmedicine.upenn.edu
Received: April 11, 2020 | Accepted: April 12, 2020 | Published: April 18, 2020
Citation: Tao H, Yang K, Gan Z, Ouyang F, Yao S, et al. Emergency Anesthesia in a Patient with Esophageal Foreign Matter Infected with COVID-19: A Case Report. Transl Perioper & Pain Med 2020; 7(3):255-257
Abstract
Anesthetic management for retrieval of the foreign matter has been well reported. But there is still no anesthetic care for patients who suffered from an Esophageal Foreign Matter (EFM) infected with coronavirus disease 2019 (COVID-19). In this case report, we present an emergency EFM patient confirmed COVID-19. Using Propofol Intravenous Anesthesia (PIA) in combination with topical anesthesia (TA), we have successfully retrieved foreign matter in the upper esophagus. Our anesthetic method supports to be an effective strategy for shortening the operation time to avoid the cross-and in-hospital SARS-CoV-2 transmission.
Keywords
Anesthetic management, Esophageal foreign matter, COVID-19, Propofol intravenous anesthesia, Topical anesthesia
Background
A recently known Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV-2) caused an outbreak of human pneumonia around the world since December 2019, which is thought to be transmitted through droplets, close contact, aerosol, and patients in the incubation period can transmit the virus to other persons [1,2]. Retrieval of Esophageal Foreign Matter (EFM) with esophagoscope is a common emergency surgery. Different sizes, shapes, and positions of foreign matter in esophagus, patients' symptoms and complex comorbidities, determines the different anesthetic management in the perioperative phase [3]. The acute anesthesia for EFM has been well established [4]. However, the anesthetic strategy for EFM patients infected with SARS-CoV-2 infection disease (COVID-19) is rare. Here we describe our experience to solve EFM by using Propofol Intravenous Anesthesia (PIA) combined with Topical Anesthesia (TA).
Case Presentation
A 48-yr-old man, admitted to Wuhan Union Hospital with EFM for 2 days, without any signs of perforation. Unfortunately, the patient suffered from a mild fever (temperature fluctuations around 37.8 ℃), dry cough and generalized fatigue for 3 days. Physical examination revealed a temperature of 37.5 ℃, BP of 135/88 mmHg, HR of 82 beats minute-1, respiratory rate of 22 bpm, and oxygen saturation (SPO2) of 96% while breathing ambient air. Bilateral lung auscultation showed no abnormalities.
A diagnosis of foreign matter ingestion was confirmed by chest computed tomography (CT), which showed an ingested fishbone in the upper esophagus (Figure 1A). Pertinent laboratory results showed lymphocyte 1.01 G·L-1, lymphocyte ratio 18.6%, and C-reactive protein 38.42 mg·L-1. Other biochemical and coagulation parameters were within normal limits. The SARS-CoV-2 detected in oropharyngeal swab samples was positive by real-time reverse transcription-polymerase chain reaction (RT-PCR) assay, whereas other viral respiratory pathogens were all negative. Chest CT showed bilateral ground-glass opacities of peripheral lungs, which are the typical manifestations of COVID-19 (Figure 1B).
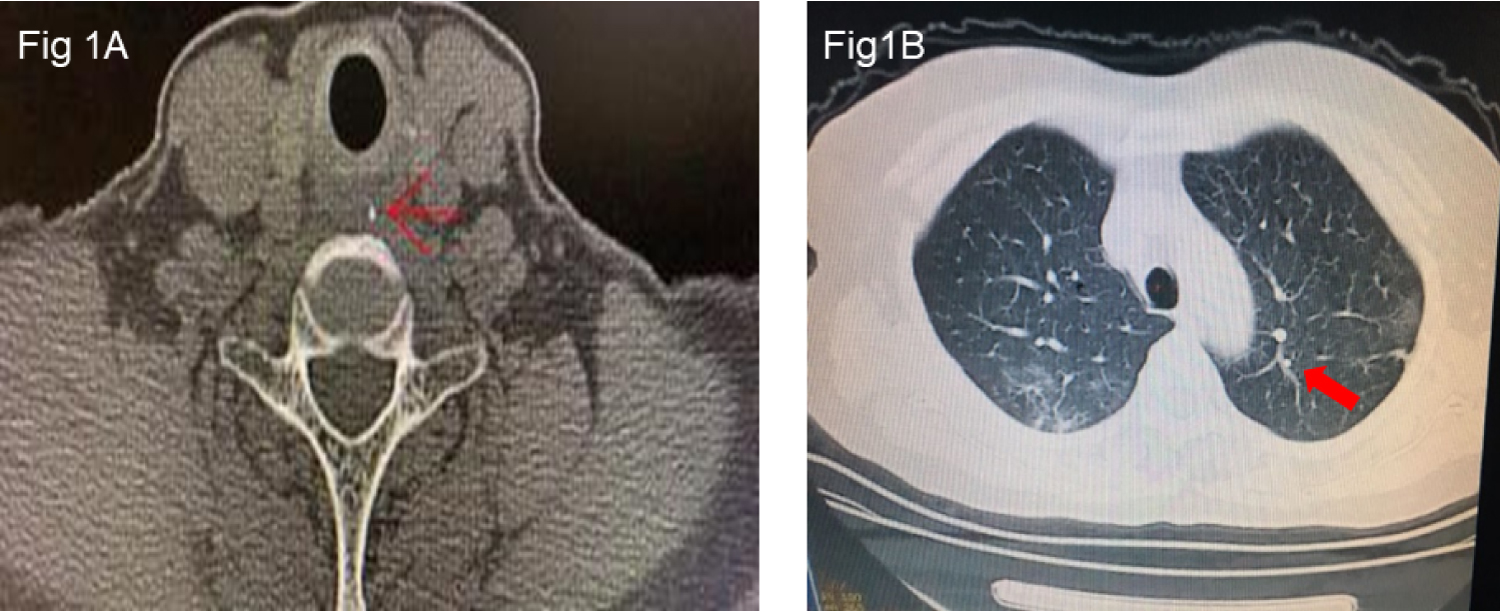
Figure 1: 1A: Foreign matter in the upper esophagus located at the position equivalent to the 7th cervical spine. Red arrows represent fishbone foreign matter. 1B: Chest CT images showed ground-glasslike shadows and patchy consolidation of bilateral lung fields.
To perform anesthesia for this COVID-19 patient, we implemented biosafety level-3 (BSL-3) measures of medical protection in the operating theatre accordingly, which included the usage of disposable protective suit, N95 medical standard face mask, disposable medical cap, medical rubber glove, goggle and face shield.
The patient was transferred to the negative pressure operating room wearing a surgical mask. Routine monitoring of the electrocardiogram, continuous non-invasive BP, SpO2, and peripheral venous catheterization were established. Nasal catheter oxygen inhalation (oxygen flow 2 L·min-1) was given under the cover of a mask. Lidocaine at 1.5 mg·kg-1 followed by propofol 2 mg·kg-1 was given intravenously. Compound lidocaine ointment was applied on the surface of the esophagoscope. The patient had a little struggle but without a cough when the esophagoscope was inserted in the esophagus, and SpO2 dropped rapidly to 75%. We immediately unblocked the airway by submaxilla-up and neck-lifting in a supine position and increased the flow of oxygen to 4 L·min-1. The surgeon halted operation concurrently for three minutes until compound lidocaine ointment worked. One minute later, the SpO2 gradually returned to 100%. We then administered an additional 50 mg propofol for the patient. After the patient's eyelash reflex had disappeared and his breath has stabilized, the esophagoscope procedure was resumed for examination. The patient vital signs remained stable for rest of the operation. The foreign matter in the esophagus was successfully removed. Five minutes after the operation, the patient's consciousness, myodynamics, and breath recovered without cough, nausea, and vomiting. After his breath has stabilized with SpO2 > 95%, the patient was transferred to the isolation ward for further treatment without any complications. SARS-CoV-2 tested among health-care workers was negative after their exposure to COVID-19 subsequently. Consent was obtained from the patient to publish this case report.
Discussion and Conclusions
Foreign matter ingestion is a relatively common emergency encounter in the field of otorhinolaryngology, which implant risks for the patients range from negligible to life-threatening with possible complications such as mucosal ulceration, esophageal perforation, and others [5,6]. However, anesthetic management for EFM patients with COVID-19 has not been reported.
COVID-19 is extremely contagious, and it has been confirmed that SARS-CoV-2 can be transmitted from person to person [2], which posed a tremendous risk for the perioperative care providers in the operating room and other perioperative settings. Except for the coverall gowns that can prevent infection by airborne pathogens, an appropriate anesthetic method for EFM removal is also crucial during the whole procedure.
TA, intratracheal intubation anesthesia, and PIA are the most common anesthetic methods for retrieval of upper EFM currently [7]. TA is the most commonly used anesthesia with low-cost for adult patients, but the patients are usually easy to struggle and bucking, which is not the priority choice for patients with COVID-19. The general anesthesia of tracheal intubation has satisfied muscle relaxation and unobstructed respiratory tract, however, it could induce or exacerbate pulmonary complications in COVID-19 patients [8]. Beyond, the risk of medical staff being exposed to aerosol transmission is greatly increased during the process of intubation and extubation. Necessary protection should be taken for both doctors and patients to prevent cross-infection. In this case, the foreign matter is relatively shallow that is located at the position equivalent to the 7th cervical spine, and it is blunt which is not easy to cause serious complications such as esophageal perforation. Thus, PIA is the preferred choice.
Simultaneously, intravenous lidocaine or topical anesthesia applied on the surface of the esophagoscope can effectively reduce the incidence of cough [9]. But be careful and wait for lidocaine to take effect before the operation. In our patient, we successfully extracted the foreign matter under PIA combined with TA.
In summary, we have described a rare case of emergency anesthetic management for retrieving foreign matter in the upper esophagus with a COVID-19 patient under propofol in combination with lidocaine anesthesia, which is proved to be an effective strategy to reduce the risk of cross- and in-hospital infection.
Competing Interests
The authors declare that they have no competing interests.
Funding
None.
Authors' Contributions
XCK contributed to writing and revising the manuscript. TH and YK contributed to performing of anesthesia. GZ and OYF contributed to the collection of data. MWK and YSL contributed to revising the manuscript. All authors read and approved the final manuscript.
Acknowledgments
The authors would like to thank the nurse anesthetists at Union Hospital in Wuhan, China for their assistance with this work.
References
- Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395:565-574. doi:10.1016/S0140-6736(20)30251-8
- Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med. 2020;382:1199-1207. doi:10.1056/NEJMoa2001316
- Abrão J, Khabbaz KM, Abrão JM, Coutinho DJ, Juliano EA. Unusual foreign body in the esophagus: a challenge for the anesthesiologist. Acta Anaesthesiol Scand. 2003;47:1176-1177. doi:10.1034/j.1399-6576.2003.00217.x
- Bao WK. Study of foreign-body extraction from the upper third of the esophagus in children. Iran J Pediatr. 2014;24:214-218.
- Li D, Nan L, Niu K, Yin W, Zhu W, Wang X. Failure of standard methods for retrieving an unusual foreign body in esophagus: A case report. Medicine (Baltimore). 2019;98:e18105. doi:10.1097/MD.0000000000018105
- Yuan J, Ma M, Guo Y, He B, Cai Z, Ye B, et al. Delayed endoscopic removal of sharp foreign body in the esophagus increased clinical complications: An experience from multiple centers in China. Medicine (Baltimore). 2019;98:e16146. doi:10.1097/MD.0000000000016146
- Geng C, Li X, Luo R, Cai L, Lei X, Wang C. Endoscopic management of foreign bodies in the upper gastrointestinal tract: a retrospective study of 1294 cases. Scand J Gastroenterol. 2017;52:1286-1291. doi:10.1080/00365521.2017.1350284
- Chen R, Zhang Y, Huang L, Cheng BH, Xia ZY, Meng QT. Safety and efficacy of different anesthetic regimens for parturients with COVID-19 undergoing Cesarean delivery: a case series of 17 patients. Can J Anaesth. 2020; doi:10.1007/s12630-020-01630-7
- Tung A, Fergusson NA, Ng N, Hu V, Dormuth C, Griesdale DGE. Pharmacological methods for reducing coughing on emergence from elective surgery after general anesthesia with endotracheal intubation: protocol for a systematic review of common medications and network meta-analysis. Syst Rev. 2019;8:32. doi:10.1186/s13643-019-0947-2