Translational Perioperative and Pain Medicine (ISSN: 2330-4871)
ARTICLE DOI: 10.31480/2330-4871/118
Case Report OPEN ACCESS
Anesthetic Management for Emergent Cesarean Delivery in a Parturient with Recent Diagnosis of Coronavirus Disease 2019 (COVID-19): A Case Report
Limin Song#, Weimin Xiao#, Ken Ling, Shanglong Yao and Xiangdong Chen*
Department of Anesthesiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430022, China
Xiangdong Chen, MD, Ph.D, Department of Anesthesiology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430022, China, Tel: +86-02785351606, Fax: +86-27-85351660, E-mail: xiangdongchen2013@163.com
Editor: Yun Xia, MD, PhD, Professor, The Ohio State University, Director, Global Health Education Initiatives, USA; E-mail: Yun.Xia@osumc.edu
Received: February 24, 2020 | Accepted: February 25, 2020 | Published: February 26, 2020
Citation: Song L, Xiao W, Ling K, Yao S, Chen X. Anesthetic Management for Emergent Cesarean Delivery in a Parturient with Recent Diagnosis of Coronavirus Disease 2019 (COVID-19): A Case Report. Transl Perioper & Pain Med 2020; 7(3):234-237.
Abstract
Corona Virus Disease 2019 (COVID-19), which was first reported in Wuhan, China in 2019, is known to cause severe respiratory infection, pneumonia and acute respiratory failure. Data on the perioperative management of pregnant women with a recent diagnosis of COVID-19 are lacking. In this case, we aim to present the anesthetic management of a 30-year-old parturient with COVID-19 who received combined spinal and epidural anesthesia during an emergent cesarean delivery.
Keywords
COVID-19, Anesthetic management, Emergent cesarean delivery, Multidisciplinary team
Background
Since December 2019, a number of cases of viral pneumonia infected with the new coronavirus, i.e. Coronavirus Disease 2019 (COVID-19), have been discovered in Wuhan, Hubei province. The pathogen causing COVID-19 was identified as 2019-nCov (https://www.who.int/emergencies/diseases/novel-coronavirus-2019). Genome sequences of 2019-nCoV revealed similarities with severe acute respiratory syndrome (SARS)-CoV and two bat-derived SARS-like coronaviruses, with whole genome sequence identities of 79% and 88%, respectively [1]. With the spread of the disease, such cases have also been found in other parts of China and abroad [2,3]. As of February 18, 2020, there are more than 72,000 confirmed cases and more than 1,850 deaths. COVID-19 is extremely contagious; recent studies demonstrate spread from person-to-person, mainly through aerosolized/aerated solids, fluids from secretions or discharges, respiratory droplets, and contact [4,5]. Though most patients who contract the virus will likely present with mild symptoms with good prognosis, some will develop severe acute respiratory infection, pneumonia, or acute respiratory distress syndrome (ARDS).
The clinical outcomes among pregnant women infected with Coronavirus are worse than their non-pregnant counterparts [6]. Anesthesiologists face difficulties with the anesthetic management of these patients during surgical procedures. Unfortunately, there is limited knowledge regarding the anesthetic management for cesarean delivery in such cases.
Here, we describe the case of a parturient with COVID-19 who underwent an urgent cesarean delivery under combined spinal and epidural anesthesia (CSEA).
Case Presentation
The study was approved by the ethics committee for clinical trials of Tongji Medical College of Huazhong University of Science and Technology, China. Written informed consent was obtained from the participant.
On February 6, 2020, a 30-year-old G5P1 female was admitted at 36 weeks and 3 days of her twin gestation to Wuhan Union Hospital, the designated institution for medical treatment of COVID-19 in Wuhan, China, for patients with confirmed diagnosis of COVID-19. The patient had a history of cesarean delivery seven years ago and no known hereditary disease. She self-reported having unprotected contact with a family member with confirmed COVID-19 diagnosis. She presented with an 8-day history of fever, cough, and generalized myalgia. Physical examination on admission revealed a temperature of 37.5 ℃, respiratory rate (RR) 22 breaths per min, blood pressure (BP) 112/70 mmHg, and heart rate (HR) 96 beats per min. There were decreased breath sounds and rales on lung auscultation. Pertinent laboratory results included hemoglobin 114 g/L, lymphocyte 1.03 G/L, lymphocyte ratio 19.4%, and C-reactive protein 34.12 mg/L. Other biochemical and coagulation parameters were within normal limits. The patient's throat swabs and fecal samples both tested positive for 2019-nCov by real-time reverse-transcription-polymerase-chain-reaction (rRT-PCR) assay, while a test of viral respiratory pathogens was negative for influenza A and B, parainfluenza, respiratory syncytial virus, mycoplasma pneumoniae, adenovirus, and coxsackievirus. Chest CT showed patchy ground glass opacities, consolidative lesions, and several fibrous stripes, mainly distributed in the subpleural regions of bilateral lungs, which is the typical manifestation of COVID-19, as shown in Figure 1. She was formally diagnosed with COVID-19 with her positive rRT-PCR result and chest CT findings. Given her diagnosis and presentation, the decision was made to perform an emergent cesarean delivery.
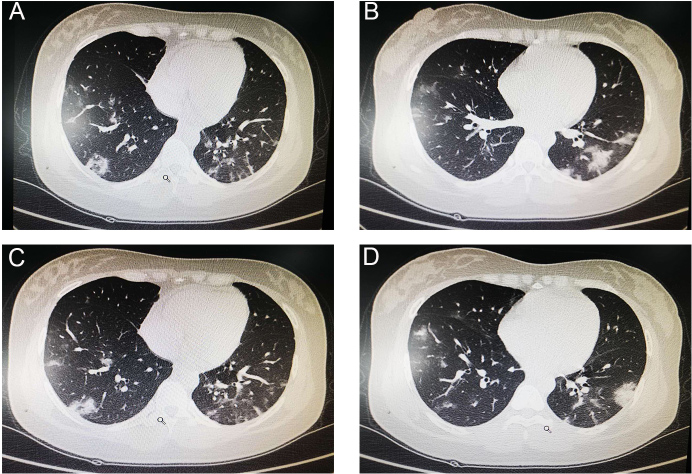
Figure 1: Chest CT findings of the patient. A-D, CT images showed multi-focal ground glass like shadows, consolidative lesions, and several fibrous stripes, predominantly involving the subpleural regions of both lungs.
The patient was transported to the operating room with a temperature of 38.5 ℃, RR 23 breaths per min, BP 112/74 mmHg, HR 81 beats per min, and oxygen saturation by pulse oximetry (SpO2) of 86-90% on room air. With the administration of oxygen via face mask at 5 L per min, her SpO2 increased to 94-96%. Peripheral venous access was obtained, and she was started on an infusion of sodium chloride. CSEA was administered in the left lateral position at the L2-3 interspace. A free-flow of cerebrospinal fluid was observed before 15 mg of 0.5% hyperbaric ropivacaine was injected and an epidural catheter was placed. Ten minutes after the spinal injection, a pinprick test was performed and the anesthetic level was found to be at the T6 level with complete motor block of the lower extremities. Fifteen minutes after the spinal injection, her BP decreased to 88/58 mmHg but returned to 110-120/64-70 mmHg after 1 mg intravenous (IV) methoxamine and infusion of additional fluids. A male baby (3.63 kg) was born 8 min after incision, with Apgar scores of 8 and 9 at 1 and 5 minutes, respectively. After delivery, 20 u of oxytocin was injected into the uterine body, as well as 12.5 mg IV dolasetron and 100 mg IV tramadol. The intraoperative blood loss was 300 ml and the patient received a total of 1000 ml of sodium chloride. Her vital signs remained stable after surgery, and she was transported to the isolation ward after removal of the epidural catheter. The neonate was also isolated in a designated unit and not breastfed.
On postoperative day (POD) 1, the patient's body temperature returned to normal and on POD 7 and 9 her rRT-PCR tests of 2019-nCoV were negative. Her newborn boy had not developed any clinical signs or symptoms of respiratory infection or compromise, and his throat swabs on days-of-life 3 and 7 were both negative for 2019-nCov RNA by rRT-PCR.
Discussion
There is limited knowledge regarding presentation and treatment of COVID-19 that occurs during pregnancy. Pneumonia during pregnancy has been proven to be associated with increased maternal and fetal morbidity and mortality. Previous experiences with respiratory infections, such as SARS and Middle East respiratory syndrome (MERS), in pregnant women indicate that these pathogens may cause severe adverse maternal and perinatal outcomes, including death [6,7]. Pregnant women with COVID-19 are considered high-risk patients, and they pose a potential anesthetic challenge during operative delivery.
It is of vital importance to avoid transmission of pathogen between patient and perioperative care providers, as well as from patient to patient. Hence, cesarean delivery of such cases should be managed in a designated negative pressure operation room. All perioperative care providers should wear protective equipment, which includes operative room scrub suits, fluid-resistant gowns, disposable gloves, eye protection, full face shield, fit-tested N95 respirators, and disposable shoe covers, as shown in Figure 2. All ventilatory circuits and anesthetic products should be discarded after surgery. Hand hygiene must be performed before and after removing protective equipment, and in the event of accidental contamination of the hands by contacting dirty surfaces during protective equipment removal [8,9].

Figure 2: All personnel wore protective equipment in the operation room. The Chinese characters on the anesthesiologist's gown (the red arrow) mean "safe and sound", which represents the aspiration of the medical staff.
These parturients require special perioperative attention as they often present with preoperative issues, such as decreased respiratory and cardiac function reserve. For this patient's hypoxia and circulatory collapse, we administered supplemental oxygen, adjusted patient positioning, and prepared vasoactive drugs in anticipation of possible hemodynamic changes.
It was reported that a newborn infant delivered on February 2, 2020 had tested positive for 2019-nCov RNA 30 hours after its birth (authors' personal communication, February 5, 2020). According to reports, the mother had been diagnosed with COVID19 before delivery. However, a recent clinical study suggests there is no evidence of vertical transmission identified among women infected with 2019-nCov in late pregnancy [10]. Amniotic fluid, cord blood, breastmilk, and neonatal throat swabs of the patients involved in this study were all negative for 2019-nCov. Based on past evidence, neonates can acquire viral infections in other ways beyond intrauterine and intra-birth canal transmission, and breastfeeding. Newborns may be infected through inhalation of contaminated aerosols and close contact with infected care providers. It is crucial to prevent infections in newborn babies born to mothers with COVID-19. The infant and all medical staff involved in our case were clinically evaluated, and none displayed evidence of COVID-19. Again, adequate personal protection and isolation significantly reduced the chances of cross-infection.
General anesthesia provides a secure airway but usually requires mechanical ventilation, which may aggravate lung injury [11]. Single-shot spinal anesthesia is a simple and flexible technique, but comes with the risk of a failed block. Therefore, we performed a CSEA to ensure adequate analgesia. CSEA offers both quick onset and reliable spinal anesthesia, coupled with the capacity to augment or prolong the blockade through an epidural catheter [12]. It can be safely applied in young pregnant women without significant comorbidities, even with maternal infection present.
Conclusion
In our case report, we describe a parturient with COVID-19 who should be comprehensively assessed before surgery. The CSEA administered in this case provided an effective anesthesia, ensured the patient's safety, and met the need for emergent cesarean delivery. Anesthetic management of such patients requires further study.
Funding
This work was supported by National Key Research and Development Project (No. 2018YFC2001802) and National Natural Science Foundation of China (NO. 81571075). No external funding or competing interests declared.
References
- Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. GenGenomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet, 2020. 395(10224): 565-574.
- Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet, 2020. 395(10223): 470-473.
- Thompson RN. Novel Coronavirus Outbreak in Wuhan, China, 2020: Intense Surveillance Is Vital for Preventing Sustained Transmission in New Locations. J Clin Med, 2020. 9(2): pii: E498. DOI: 10.3390/jcm9020498.
- Lu CW, Liu XF, Jia ZF. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet, 2020. 395(10224): e39. DOI: 10.1016/S0140-6736(20)30313-5
- Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med, 2020. DOI: 10.1056/NEJMoa2001316.
- Wong SF, Chow KM, Leung TN, Ng WF, Ng TK, Shek CC, et al. Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. Am J Obstet Gyneco, 2004. 191(1): 292-297.
- Abdullah A, Abedi GR, AI Masri M, Bin Saeed A, Gerber SI, Watson JT. Middle East Respiratory Syndrome Coronavirus Infection During Pregnancy: A Report of 5 Cases From Saudi Arabia. Clin Infect Dis, 2016. 63(7): 951-953.
- Zamora JE, Murdoch J, Simchison B, Day AG. Contamination: a comparison of 2 personal protective systems. CMAJ, 2006. 175(3): 249-254.
- Chen X, Shang Y, Yao S, Liu R, Liu H. Perioperative Care Provider's Considerations in Managing Patients with the COVID-19 Infections. Perioper & Pain Med, 2020. 7(2): 216-223.
- Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet, 2020. DOI: https://doi.org/10.1016/S0140-6736(20)30360-3.
- Ding X, Tong Y, Jin S, Chen Z, Li T, Billiar TR, et al. Mechanical ventilation enhances extrapulmonary sepsis-induced lung injury: role of WISP1-αvβ5 integrin pathway in TLR4-mediated inflammation and injury. Crit Care, 2018. 22(1): 302. DOI: 10.1186/s13054-018-2237-0
- Wang Y, Xu M. Comparison of ropivacaine combined with sufentanil for epidural anesthesia and spinal-epidural anesthesia in labor analgesia. BMC Anesthesiol, 2020. 20(1): 1. DOI: 10.1186/s12871-019-0855-y.